Mpox : Where else can you find Mpox? Explained
677
Mpox is an uncommon condition produced by the Mpox virus that resembles smallpox. While it has been spotted in other parts of the world, it is mostly prevalent in parts of Africa. It causes flu-like symptoms such as fever, chills, and a rash that may take weeks to go away. Despite having no known treatment, Mpox frequently goes away on its own.
The rare disorder known as Mpox is brought on by the Mpox virus. It results in a rash and flu-like symptoms. It belongs to the same family as the more well-known smallpox virus, the orthopoxviruses.
Two outbreaks of a condition mimicking pox in groups of monkeys used for research resulted in the identification of Mpox in 1958. Rodent contact with sick people accounts for the majority of the disease's transmission, while skin-to-skin contact with an infected person can occasionally transfer the infection. One lineage of the Mpox virus originated in Central Africa, whereas the other one did so in West Africa. The current worldwide pandemic originated in the less hazardous West African lineage (2022).
Mpox is a rare illness. But, incidences are increasing in Africa and other regions that have not historically seen the same illnesses.
Where else can you find Mpox?
The majority of Mpox cases for many years were in Africa. Yet, it does occasionally occur in other countries, such as the United States. The country saw its first Mpox epidemic outside of Africa in the spring of 2003. Texas got a shipment of sick animals from Ghana. The tamed prairie dogs that the ill rodents passed the virus to eventually infected 47 people in the Midwest.
As international travel becomes more commonplace, viruses that were formerly primarily confined to local regions may spread more quickly around the world. A U.S. citizen who had traveled to the nation from Nigeria was found to have Mpox in the summer of 2021. Eventually, in 2022, infections expanded to non-African regions including Europe, the Americas, and Australia.
Everyone may contract Mpox. In Africa, children under the age of 15 are involved in the majority of instances.
Causes
Mpox can spread from one person to another by way of:
- Any close physical contact with blisters or scabs from a Mpox infection (including during sexual contact, kissing, cuddling or holding hands)
- Coughing or sneezing of an individual with Mpox while they are close to you touching items, bedding, or towels used by an individual with Mpox
Mpox may also be contracted by infected rodents (such as rats, mice, and squirrels) in several regions of west and central Africa if:
- When you contact with their skin, fur, blood, bodily fluids, spots, blisters, or scabs, you become bitten.
- You consume their meat, which has not been properly prepared.
Symptoms
The onset of symptoms following exposure might be days or even weeks away. First signs of measles include flu-like symptoms like:
- Fever.
- Chills.
- Headache.
- Muscular pain.
- Fatigue.
- Lymph nodes with swelling.
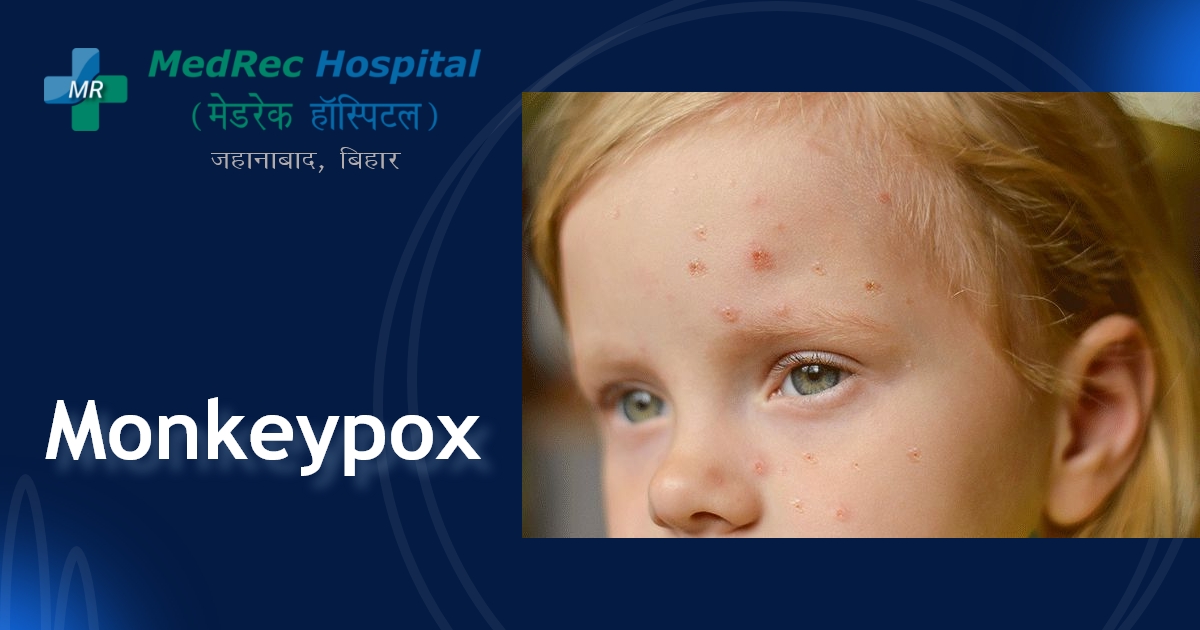
Many times, a rash develops a few days later. The first signs of the rash are uncomfortable, flat, and red pimples. These lumps grow into pus-oozing blisters. It usually takes two to four weeks for the blisters to harden over and peel off. Moreover, oral, vaginal, or anus ulcers are possible.
Not every patient with Mpox experiences every symptom. In fact, many patients in the current (2022) outbreak are not exhibiting the typical constellation of symptoms. There are just a few lesions in this unusual appearance, no enlarged lymph nodes, and decreased illness-related symptoms like fever. You may possess it without realizing it. Even if you do not show many signs of the virus, you can still spread it to other people if you stay in close proximity to them for a long time.
How can one capture pox?
You might contract Mpox if you come in contact with a person or animal that has the virus. By biting or scratching people, or by coming into contact with their blood, bodily fluids, or lesions from an afflicted animal, animals can spread illnesses to people (sores).
Mumps can spread from person to person even though it does so less frequently. Person-to-person transmission occurs when you come into contact with the sores, scabs, respiratory droplets, or oral secretions of a sick person, usually in close, private settings (transmission).
Moreover, you can get Mpox by touching recently contaminated items like the clothing, bedding, and other linens used by an infected person or an infected animal.
Prevention
The use of a smallpox vaccination, which protects against Mpox, is now restricted to clinical studies. Preventive measures include limiting person-to-person transmission and minimizing human contact with sick animals. The best strategy to stop the Mpox virus from spreading is to:
- Avoid touching ill animals (especially sick or dead animals).
- Avoid coming into contact with contaminated bedding and other items.
- Cook all items containing meat or other animal products completely.
- Cleanse your hands with soap and water on a regular basis.
- Maintain a safe distance from someone who could be a virus carrier.
- Use safe sexual practices, such as the use of dental dams and condoms.
- While among other people, wear a mask that covers your mouth and nose.
- Surfaces that are touched often need to be cleaned and sanitized.
- Wear personal defense tools (PPE) when tending to those who have the illness.
Treatments
Mpox often has symptoms that last between two and four weeks and is a self-limiting illness. Most Mpox sufferers recover on their own without medical intervention. With a diagnosis, your doctor will keep an eye on your health, try to alleviate your symptoms, avoid dehydration, and administer antibiotics to treat any developing secondary bacterial infections.
With Mpox, there is not yet an authorized antiviral medication. While they have not been researched as a Mpox therapy, antiviral medications may be helpful. There are a number of experimental antivirals with action against Mpox, however, they can only be obtained in a research trial.
There are over-the-counter medicines that can help you feel better if you suffer symptoms of Mpox, including:
Anti-fever medications and painkillers. You may feel better after taking medications like acetaminophen (Tylenol®) and ibuprofen (Advil®, Motrin®).
Almond baths. The dry, itchy sensation that occurs with skin rashes can be relieved by soaking in a warm bath with colloidal muesli.
If you have the disease, isolate yourself. Wait until all of your sores have scabbed before making contact with people.
Include limited or isolated lesions. To prevent the transmission to other people and the environment, use gauze or bandages.
Please be careful. When you are unwell, it is crucial to relax at home, cover your face around other people, and drink lots of water.
Stay away from pets (especially rodents).
Mpox is typically a benign condition, and most patients recover on their own in a few weeks.
But, if your symptoms worsen and you start to feel ill, you could need medical care.
The likelihood of requiring hospital care is increased for:
- People who are older, younger, suffering from an illness, or taking medication that impairs their immune system
- If you have the virus, it is crucial to separate yourself since it might spread through close contact. If your symptoms are minor, you could be instructed to isolate yourself at home.
Complications of Mpox
Mpox typically takes two to four weeks to complete its course. Your provider will keep an eye on you if you have been exposed to Mpox until the rash goes away.
The current global outbreak is being caused by the less dangerous West African lineage (2022). This epidemic has not yet resulted in any fatalities. Nevertheless, Mpox can cause other issues (complications), including pneumonia and potentially deadly encephalitis and eye or brain infections.
For further information please access the following resources:
Emergency : +91 89686 77907
Front Desk : +91 98018 79584
Page last reviewed: Mar 29, 2023
Next review due: Mar 29, 2025







.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)