Multiple Sclerosis : How to check if you have Multiple Sclerosis?
701
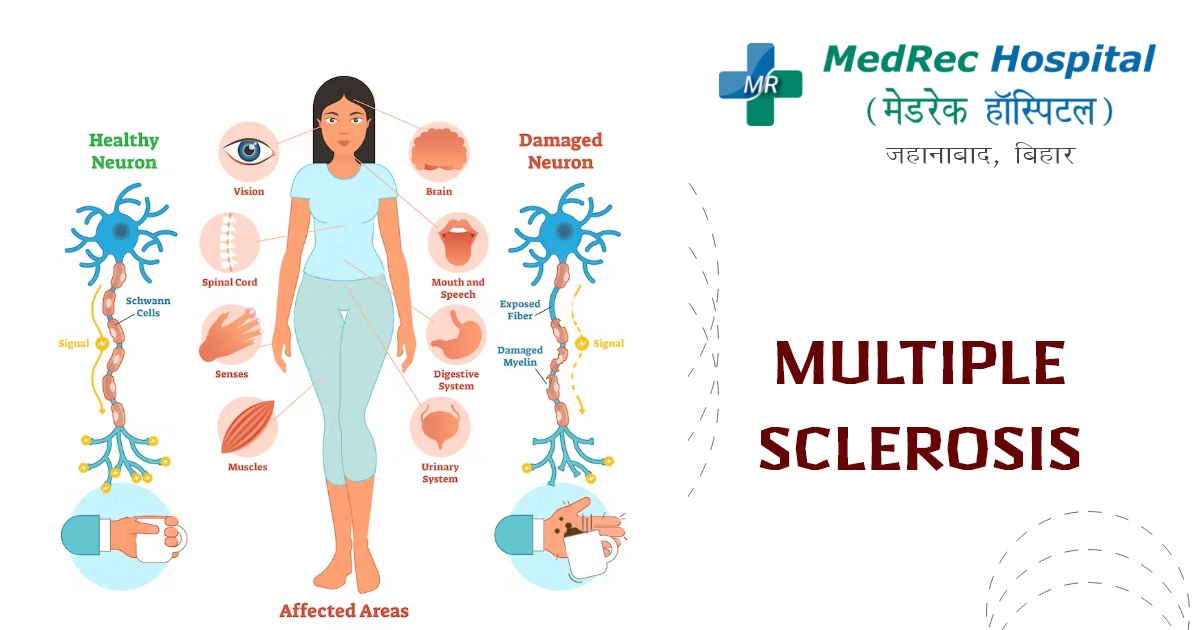
It is possible for multiple sclerosis (MS) to disable the brain and spinal cord (central nervous system).
Myelin, the protective coating that protects nerve fibers, is attacked by the immune system in MS, which impairs brain-to-body communication. The condition may eventually result in nerve fiber degeneration or irreversible injury.
The location and degree of nerve fiber damage in the central nervous system affects the signs and symptoms of MS, which vary greatly from patient to patient. Some MS patients may lose their ability to walk independently totally or in part. Depending on the type of MS they have, other people could go for extended stretches of time without developing any new symptoms.
Multiple Sclerosis has no known treatment option. However, treatments are available to slow the onset of episodes, alter the course of the illness, and control symptoms.
Health condition
The majority of MS patients experience relapsing-remitting illness. They go through phases of developing new symptoms or relapsing that take days or weeks to develop and often get well partially or entirely. After these relapses, there may be months or even years of calm illness remission.
Modest changes in body temperature have the potential to temporarily exacerbate MS symptoms. They are regarded as pseudo relapses rather than actual illness relapses.
Within 10 to 20 years of the commencement of the illness, 20% to 40% of people with relapsing-remitting MS might eventually experience a constant development of symptoms, with or without remission intervals. MS with secondary progression is what this is.
Mobility and gait issues are frequently present with increasing symptoms. The rate of illness development varies significantly in MS patients with secondary-progressive disease.
Primary-progressive MS, which affects certain persons with the disease, is characterized by a slow beginning and continuous progression of signs and symptoms without any relapses.
Causes
Multiple sclerosis does not have a recognised etiology. When the immune system of the body targets its own tissues, an illness known as immune mediated is the result. The fatty material that covers and shields the nerve fibers in the brain and spinal cord in MS is destroyed by this immune system error (myelin).
Myelin is comparable to the insulating layer that covers electrical cables. The messages that go along that nerve fiber may be slowed down or inhibited when the protecting myelin is broken and the nerve fiber is exposed.
Why some people acquire MS and others do not is unclear. It seems that both inherited and environmental factors are involved.
How to check if you have Multiple Sclerosis?
If you encounter any of the symptoms listed above for an unidentified reason, consult a doctor.
Risk Factors
Some elements might make you more likely to have multiple sclerosis:
Age. MS can strike at any age, however the average onset age is between 20 and 40. Yet, both young and elderly might be impacted.
Sex. Relapsing-remitting MS affects more than 2 to 3 times as many women as it does males.
Family background. You have an increased chance of getting MS if one of your parents or siblings has the condition.
Certain infections. Several viruses, including Epstein-Barr, the virus that causes infectious mononucleosis, have been connected to MS.
Race. The chance of acquiring MS is higher among white persons, particularly those of Northern European heritage. The lowest risk groups are those with Asian, African, or Native American ancestry. Recent research shows that there may be more young individuals with multiple sclerosis in the Black and Hispanic communities than previously believed.
Climate. In nations with temperate temperatures, such as Canada, the northern United States, New Zealand, southeastern Australia, and Europe, MS is far more prevalent. Although exposure to the sun when a mother is pregnant appears to reduce the later development of multiple sclerosis in these children, your birth month may also have an impact on your risk of acquiring multiple sclerosis.
Calcium D. Low vitamin D levels and little sun exposure are linked to an increased risk of MS.
The genetics. Multiple sclerosis has been connected to a gene on chromosome 6p21.
Obesity. In females, there is a connection between obesity and multiple sclerosis. This is particularly true for female teenage and childhood obesity.
Certain autoimmune conditions. If you have other autoimmune diseases including thyroid disease, pernicious anaemia, psoriasis, type 1 diabetes, or inflammatory bowel disease, your chance of having MS is somewhat increased.
Smoking. Smokers are more likely than non-smokers to encounter a second episode that confirms relapsing-remitting MS after experiencing a first symptom that may indicate MS.
Symptoms
The signs and symptoms of multiple sclerosis can differ greatly from person to person and during the course of the disease depending on where the damaged nerve fibers are situated.
Typical signs include:
- It affects one side of your body at a time, numbness or weakness in one or more limbs
- Some neck motions, notably bending the neck forward, might cause tingling electric-shock feelings (Lhermitte sign)
- Ineffective coordination
- Incapacity to walk or an unsteady stride
- Partial or total blindness, generally affecting just one eye at a time, frequently accompanied by discomfort when moving the eye
- Long-lasting double vision
- Hazy vision
- Vertigo
- Issues with bowel, bladder, and sexual function
- Fatigue
- Unsteady speech
- Cognitive difficulties
- Disturbances in mood
Treatments
Multiple Sclerosis has no known treatment option. The main goals of treatment for MS are to manage symptoms, limit the disease's development, decrease new radiological and clinical relapses, and hasten recovery from attacks. Some people simply display modest symptoms, requiring only minimal medical care.
Treatments for MS attacks
To minimize nerve irritation, doctors often administer corticosteroids such as oral prednisone and intravenous methylprednisolone. Possible adverse effects include fluid retention, insomnia, high blood pressure, high blood sugar, and mood swings.
Exchange of plasma (plasmapheresis). Your blood is extracted, and the liquid plasma is separated from the blood cells. The blood cells are then returned into your body after being mixed with albumin, a protein solution. After undergoing steroid therapy, if your symptoms are new, severe, and not getting better.
Therapies to slow progression
Several disease-modifying treatments (DMTs) are available for relapsing-remitting MS. One of these DMTs is available for primary progressive MS, and some of them may be helpful for secondary progressive MS.
Most of the MS immune response starts early in the course of the illness. Early and aggressive use of these drugs can minimize the recurrence rate, limit the growth of new lesions, and perhaps lessen the risk of brain atrophy and disability accumulation.
Significant health hazards are associated with several of the disease-modifying treatments used to treat MS. The optimal therapy for you will rely on carefully weighing a variety of criteria, such as the length and severity of the illness, the success of prior MS therapies, additional medical conditions, cost, and whether or not you are a parent.
Injectable, oral, and infusion medicines are available for relapsing-remitting MS.
Among the injectable therapies are:
- Drugs containing interferon beta. The majority of MS patients were treated with these meds in the past. They function by preventing pathogens from attacking
- The body might promote the creation of new nerves while reducing inflammation. They are injected into the muscle or beneath the skin, and they can lessen the number and severity of relapses.
- Flu-like symptoms and injection site responses are possible. As liver damage is a potential adverse effect of using interferon, blood tests will be necessary to monitor your liver enzyme levels. Interferon users may produce neutralizing antibodies that might lessen the efficiency of the medicine.
- Acetate of glatiramer (Copaxone, Glatopa). This medicine, which needs to be injected under the skin, may help prevent your immune system from attacking your myelin. Skin inflammation at the injection site is one of the potential side effects.
- Antigens that are monoclonal. Ofatumumab (Kesimpta, Arzerra) targets nerve-damaging cells in the body. B cells are the name for these cells. It is administered by a skin injection and can lessen the progression of multiple sclerosis symptoms and brain lesions. Infections, localized injection-related responses, and headaches are all potential adverse effects.
Oral remedies consist of:
Teriflunomide (Aubagio). This oral drug, taken once daily, can lower the recurrence rate. Other negative effects of teriflunomide include liver damage and hair loss. Both men and women who use this medication run the risk of having children with birth abnormalities. Hence, for up to two years after stopping this drug, utilize contraception. If a couple wants to get pregnant, they should see their doctor about techniques to hasten the drug's removal from the body. Regular blood test monitoring is necessary for this medication.
Fumarate of dimethyl (Tecfidera). This oral drug, taken twice daily, can lessen relapses. The potential negative consequences of diarrhea, nausea, and a decreased white blood cell count are other symptoms. Regular blood test monitoring is necessary for this medication.
Fumarate of diroxime (Vumerity). Similar to dimethyl fumarate, but usually with fewer side effects, is this twice-daily pill. It has been given the go-ahead to treat relapsing types of MS.
Flushing, liver damage, stomach discomfort, and infections are possible adverse effects.
Fingolimod (Gilenya). The recurrence rate is decreased by this once-daily oral drug.
As your heart rate can be reduced after the first dosage, you will need to have your blood pressure and heart rate checked for six hours after that.
Additional adverse effects include headaches, high blood pressure, uncommon but deadly infections, and impaired vision.
Siponimod (Mayzent). This once-daily oral medicine has been shown in studies to help slow the course of MS and minimize relapse rates. Moreover, secondary-progressive MS is accepted for use. Viral infections, liver issues, and low white blood cell count are examples of potential adverse effects. Additional negative effects including variations in heart rate, headaches, and eyesight issues. Women who may get pregnant should use contraception while taking siponimod and for 10 days after discontinuing it since it is detrimental to a developing baby. Some people might require six hours of blood pressure and heart rate monitoring following the initial dosage. Regular blood test monitoring is necessary for this medication.
Ozanimod (Zeposia).
This once daily oral medicine reduces the recurrence rate of multiple sclerosis. Infections, liver inflammation, and high blood pressure are examples of potential adverse effects.
Ponesimod (Ponvory). This oral drug has a once-daily dose plan that progressively increases. This drug is shown to cause less brain lesions than certain other multiple sclerosis treatments and has a low recurrence rate. Infections of the respiratory tract, excessive blood pressure, irritation of the liver, and issues with the electrical activity of the heart can all be adverse effects.
Cladribine (Mavenclad). For those with relapsing-remitting MS, this drug is typically administered as a second line of therapy. Moreover, it was authorized for secondary-progressive MS. It is administered during two therapy sessions, separated by a two-week period. Headaches, malignancies, severe infections, and decreased numbers of white blood cells are a few of the side effects. Those who are pregnant or nursing should not use this medication, nor should those who have active malignancy or chronic illnesses. For the first six months of using this drug, both men and women should utilize birth control. When using cladribine, you might require blood tests for monitoring.
Infusion therapies consist of:
Natalizumab (Tysabri). It has been demonstrated that this monoclonal antibody lowers recurrence rates and lowers the likelihood of impairment.
The goal of this drug is to prevent potentially harmful immune cells from traveling from your circulation to your brain and spinal cord. That may be regarded as a first or as a second- or third-line therapy for some patients with severe MS.
In patients who have antibodies to the virus that causes PML JC, progressive multifocal leukoencephalopathy (PML), this drug raises the risk of a potentially severe viral infection of the brain. The likelihood of developing PML in those without the antibodies is quite low.
Ocrelizumab (Ocrevus). In relapsing-remitting multiple sclerosis, this medication lowers the relapse rate and the chance of debilitating progression. Moreover, it reduces the course of multiple sclerosis' primary-progressive variant.
A healthcare provider administers ocrelizumab by intravenous infusion. There are a number of side effects associated with infusions, including itchiness at the injection site, low blood pressure, fever, and nausea. Ocrelizumab may not be suitable for everyone, particularly individuals with hepatitis B infections. Ocrelizumab may also make some cancers, notably breast cancer, and infections more likely.
Alemtuzumab (Campath, Lemtrada). This medication, a monoclonal antibody, lowers yearly recurrence rates and shows MRI advantages.
By attacking a protein on the surface of immune cells and decreasing white blood cells, this medication helps prevent MS relapses. This result can reduce the risk of nerve injury brought on by the white.
Red blood cells. Yet it also raises the risk of infections and autoimmune illnesses, such as uncommon immune-mediated kidney disease and thyroid autoimmune diseases, which are both highly risky.
A year later, further three days of infusions are administered as part of the alemtuzumab course of treatment. Alemtuzumab infusion reactions are frequent.
Drug users are required to register in a unique drug safety monitoring scheme, and the medication is only sold by licensed providers. For individuals with active MS or as a back-up treatment if another MS drug fails, alemtuzumab is typically advised.
New discoveries or emerging treatments
A new treatment for secondary-progressive multiple sclerosis and relapsing-remitting multiple sclerosis is Bruton's tyrosine kinase (BTK) inhibitor. It operates by B cells, immune cells found in the central nervous system, are mostly modulated.
The immune system of a patient with multiple sclerosis is destroyed during stem cell transplantation, and the patient's immune system is subsequently replaced with healthy stem cells. The potential for this treatment to lessen inflammation and "reset" the immune system in MS patients is currently being researched. Fever and infections are potential adverse effects.
Researchers are learning more about how current disease-modifying medicines function to diminish relapses and lessen lesions in the brain caused by multiple sclerosis. If a therapy may postpone the disease's impairment, further research will be needed to make that determination.
Treatments for the symptoms and indicators of MS
Multiple sclerosis physical therapy
Muscle strength can be increased through physical treatment, which can also reduce some MS symptoms.
Therapy. You can learn stretching and strengthening exercises from a physical or occupational therapist, and they can also demonstrate how to utilise equipment to make daily activities simpler.
Leg weakness and other gait issues frequently linked with MS can also be managed with physical therapy and the use of a mobility device, if needed.
Muscles relaxants. You might feel severe or uncontrolled leg-specific muscular stiffness or spasms. Muscle relaxants such cyclobenzaprine, tizanidine, and baclofen (Lioresal, Gablofen) may be helpful. Onabotulinumtoxina is another choice for persons with spasticity/
Drugs that lessen weariness. MS-related tiredness has been treated with amantadine (Gocovri, Osmolex), modafinil (Provigil), and methylphenidate (Ritalin). Nevertheless, a recent trial found that amantadine, modafinil, or methylphenidate did not improve MS-related tiredness better than a placebo and produced more side effects. Selective serotonin reuptake inhibitors are among the medications used to treat depression that could be suggested.
Medication to quicken walking. Some persons may benefit from a minor increase in walking pace when taking dalfampridine (Ampyra). Urinary tract infections, vertigo, sleeplessness, and migraines are all potential adverse effects. Not recommended for those with a history of seizures or renal disease.
Different medicines. Moreover, MS-related depression, discomfort, sexual dysfunction, sleeplessness, and issues with bladder or bowel control may be treated with medication.
Complications of Multiple Sclerosis
Multiple sclerosis patients may also experience:
- Muscle spasms or stiffness
- Severe lassitude or paralysis, usually affecting the legs
- Issues with the bowels, bladder, or sexual function
- Cognitive issues, such as forgetfulness or trouble finding words
- Depression, anxiety, and mood swings are examples of mood disorders
- Seizures are quite infrequent.
For further information please access the following resources:
Emergency : +91 89686 77907
Front Desk : +91 98018 79584
Page last reviewed: Mar 29, 2023
Next review due: Mar 29, 2025







.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)